Nephrotic syndrome is a disease characterized by the appearance of blood in the urine (hematuria), elevated blood pressure (high blood pressure) and an acute renal function failure that causes the child to urinate less, and retain fluid and swell (edema). All these alterations may appear together or not and to varying degrees.
Why does it occur?
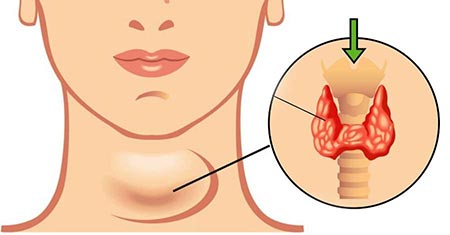
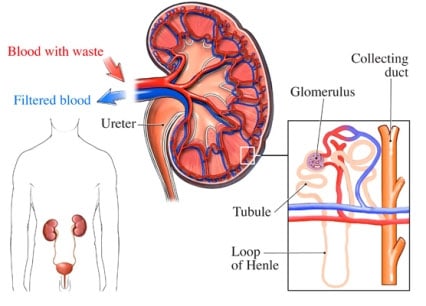
The nephrotic syndrome occurs because the kidney becomes inflamed, specifically internal structures called glomeruli that act as a filter or strainer. This inflammation of the glomerulus (glomerulonephritis) usually occurs after an infection, such as angina or skin infection caused by a bacterium called streptococcus (acute post-streptococcal glomerulonephritis).
It is not a kidney infection but occurs as a result of inflammatory response after infection. Other times, the glomerulus is altered without a known cause (primary glomerulonephritis) or by diseases that affect other parts of the body, such as in systemic lupus erythematosus, or IgA nephropathy (immunoglobulin A).
Symptom
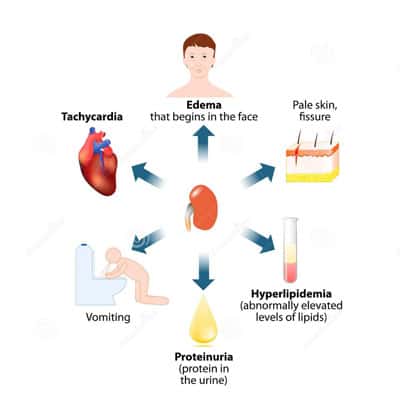
Common symptoms of nephrotic syndrome are:
- Blood in the urine (dark, tea-colored or cloudy urine)
- Decreased urine volume (little or no urine may be produced)
- Swelling of the face, orbits, legs, arms, hands, feet, abdomen or other areas
- High blood pressure
Other symptoms that may occur include:
- Blurred vision, usually because of a blood vessel in the retina of the eye that bursts
- Cough that contains mucus or foamy and pink material because of the accumulation of fluid in the lungs
- Trouble breathing, because of the accumulation of fluid in the lungs
- General malaise (indisposition), drowsiness, confusion, aches and pains, headache Symptoms of acute renal failure or prolonged (chronic) kidney disease may occur.
Other Symtoms
The way in which the nephrotic syndrome manifests is very variable because not all the symptoms always appear together and in the same way. Blood in the urine (hematuria), for example, may be visible to the naked eye, with red or brown urine appearing, such as in meat washing water (macroscopic hematuria) and other times it can only be seen by scanning the urine with a microscope ( microscopic hematuria). Characteristically, the child does not feel any pain.
The alteration of renal function may be more or less intense, the child may urinate somewhat less or almost nothing and the edema may be very obvious or subtle. Blood loss in the urine can be accompanied by proteinuria (loss of protein in the urine), which increases edema (swelling). They can appear on the eyelids, legs, ankles or be generalized and cause the weight to increase. Sometimes children complain of a headache (especially if they have high blood pressure) and are tired.
Diagnosis
The diagnosis is suspected by symptoms and exploration. To confirm this, a urine test must be performed in which hematuria with or without proteinuria and a blood test to assess renal function will be observed. Depending on the previous history and the clinical history, other tests will be requested to try to find the cause: pharyngeal or skin culture, immunological tests (antibodies involved in the alteration of the glomerulus). In highly selected cases, a renal biopsy (analysis of a kidney sample) is necessary to find out the cause and severity of the renal involvement.
Treatment
There is no specific treatment for nephrotic syndrome. The objective is to control the alterations that it produces until the disease remits spontaneously:
- It is recommended not to abuse salt. If there are edema and/or arterial hypertension, a salt-free diet must be performed and the fluid intake reduced.
- Sometimes treatment with diuretics (medicines to urinate more) is needed to get edema and hypertension to decrease.
- In the most severe forms that do not remit spontaneously, sometimes the use of corticosteroids and even other immunosuppressants are required (to control the immune response that is damaging the kidney) depending on the cause.
Expectations (prognosis)
The prognosis depends on the disease that is causing the nephritis. When the condition improves, fluid retention symptoms (such as edema and cough) and high blood pressure may disappear in 1 or 2 weeks. Urine tests take months to return to normal. Children tend to have a better prognosis than adults and usually recover completely. Only rarely do
they suffer complications or aggravate and progress to chronic glomerulonephritis and chronic kidney disease.
Adults do not recover as well or as fast as children. Although it is unusual for the disease to come back, in some adults acute nephrotic syndrome does return, and this group will have end-stage renal disease and may need dialysis or kidney transplantation.



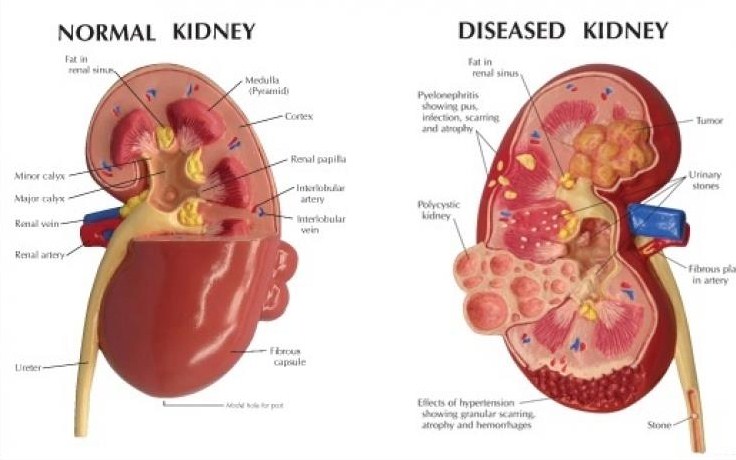



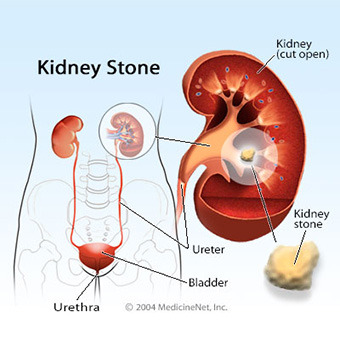
 Pyelonephritis is a potentially serious infectious inflammatory disease caused by bacteria. It affects the renal parenchyma, where the urine-producing functional structures are located, and the dilated portion of the kidney (or pelvis), roughly shaped like a funnel, whose function is to facilitate the flow of urine through the ureters. so that it is stored in the bladder and then eliminated through the urethra.
Pyelonephritis is a potentially serious infectious inflammatory disease caused by bacteria. It affects the renal parenchyma, where the urine-producing functional structures are located, and the dilated portion of the kidney (or pelvis), roughly shaped like a funnel, whose function is to facilitate the flow of urine through the ureters. so that it is stored in the bladder and then eliminated through the urethra.